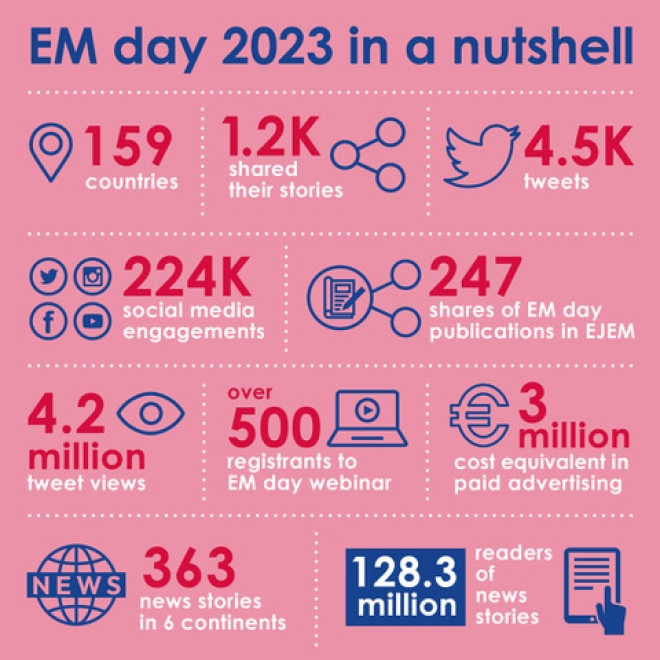
EM Day international survey on patient safety published in the European Journal of Emergency Medicine
For EM-Day 2023 we conducted 3 surveys about safety, for patients/general public, for professionals and for patient organisations.
The survey (1) included 1256 responses from 101 different countries; 70% of respondents were from Europe. Among respondents, 80% reported that monitoring devices were available, and 74% reported that protocols for high-risk medication and for triage (66.19%) were available in their ED. The area of greatest concern was the disproportionate imbalance between needs and the availability of staff at times of greatest flow, considered sufficient by only 22% of doctors and 20% of nurses. Other critical issues were overcrowding due to boarding and a perceived lack of support from hospital management. Despite these difficult working conditions, 83% of the professionals said they were proud to work in the ED. This survey highlighted that most health professionals identify the ED as an environment with specific safety issues. The main factors appeared to be a shortage of personnel during busy periods, overcrowding due to boarding, and a perceived lack of support from hospital management. The results were published in the European Journal of Emergency Medicine.
Dr Jim Connolly, EUSEM president writes in his editorial (2): "Amongst the headline results the authors found that about 90% of professionals feel that at times the number of patients in their ED exceeded the capacity of the department to provide safe care and that overcrowding was currently a regular, serious problem. Overcrowding is not just an issue of discomfort or loss of dignity but adds to inefficiency and carries a substantial risk of harm and increased mortality"
Read further:
(1) Patient safety in emergency departments: a problem for health care systems? An international survey
Press Release: Are Emergency Departments unsafe? Patients and professionals think so
Emergency departments (EDs) are currently unsafe places for both professionals and patients, according to the results of an international survey carried out for the European Society of Emergency Medicine (EUSEM) and published today (26th May) in the European Journal of Emergency Medicine1. The main reasons for this are staff shortages and overcrowding due to the non-availability of beds in wards necessitating the provision of care in corridors. Respondents to the survey also felt that they had insufficient support from hospital management.
Around 90% of professionals surveyed felt that at times the number of patients in ED exceeded the capacity of the department to provide safe care, and that such overcrowding was a regular problem. In addition to causing patient and professional discomfort and impeding their ability to provide care, overcrowding is known to carry a substantial risk of harm and increased mortality.
The preliminary findings of a survey among patients, yet to be published, were even more alarming. More patients thought that ED staff were ‘angry’ or ‘rude’ than were kind. This is likely to be caused by exhaustion and frustration, says an accompanying editorial2 from EUSEM President Dr James Connolly ‘given that the vast majority of those responding to the survey of professionals said that they were proud to work in an ED.’ Amongst responses received a typical response was “There were a lot of patients and very few doctors. Some nurses were very stressed.”
Indeed, nurses who responded to the survey felt less safe than did doctors, particularly with regards to the environment in which they had to treat patients with mental health problems. Since in general they work with patients for longer periods of time, this is understandable, but nonetheless troubling, say the researchers.
“Last year’s EUSEM survey into burnout among ED professionals was worrying enough,” says Dr Connolly, “showing as it did that younger and less experienced EM professionals were more likely to be affected than older, more experienced staff. It is very disquieting to see this pattern repeated, and completely unacceptable that so little action has been taken to remedy it. If anything, the situation appears to be worse than before.” This is especially important, as In many EDs the majority of professionals are still junior and therefore at greater risk of burnout, and so in greater need of supervision to protect both themselves and their patients.
Although targets have been advantageous in bringing about improvements in the past, the current feedback from ED staff shows that, when systems are under significant strain, they feel pressurised by the imposition of such external targets, and that they believe this could cause patient care to suffer. Some 54.2% said they were permanently under external pressure. Support from hospital management was also perceived to be inadequate; 35% of professional responders responding that hospital managers never supported the introduction of improvements, and 47% thinking that procedures for improving flow in the ED were never effective.
Alarmingly, some patients surveyed felt so concerned about their safety in the ED that they said they would prefer not to go there at all, believing that overcrowding, long waiting times, and exhausted staff would lead to medical errors.
“Dedicated professionals need the right environment and support in which to carry out their work, and patients need to feel reassured that they will get the best treatment. Currently we are far from that being the case. Governments and healthcare authorities must remedy this now, before the situation worsens further when it may become too late to arrest the spiral of decline,” says Dr Connolly.
1. https://journals.lww.com/euro-emergencymed/Abstract/9900/Patient_safety_in_emergency_departments__a_problem.63.aspx
DOI 10.1097/MEJ.0000000000001044
2. https://journals.lww.com/euro-emergencymed/Citation/9900/With_safety_in_mind.64.aspx
DOI 10.1097/MEJ.0000000000001048
Further information:
Davi Kaur
Email: This email address is being protected from spambots. You need JavaScript enabled to view it.
Mobile: +32 485515497
It's almost EM-Day!!
This week the EUSEM website is showing the EM-Day, 27 May, colours. We are very excited about all the submissions in the web-app and the activities that are coming in through This email address is being protected from spambots. You need JavaScript enabled to view it.
The map of impact is already looking amazing with activities from all over the world!
Even though EM-Day is on the 27th, the 26th of May will be also a big day for EUSEM and the EM-Day team.
- The paper and editorial about the survey results will be published in the European Journal of Emergency Medicine. The press release will be showing on the EUSEM homepage linking to the publications. Fingers crossed for a lot of media attention!
- The webinar: Safety Culture in the ED will be held at 14:00 CEST. The survey results will be presented and we have great speakers representing WHO, IAPO, IFEM, AFEM, EUSEM and more. We will exchange thoughts and ideas about improving the safety in the ED. Please register and join the round table discussion.
Please join in the campaign and tag us on the socials and add the hashtags #YourSafetyOurPriority #EmergencyMedicineDay
Fb: @EmergencyMedicineDay
Tw: @EmergencyDay
Insta: emergency_day\
In: company/emergency-medicine-day
Acute CV Days: Everything you need to know about acute myocardial infarction
AcuteCVDays facilitates learning and discussing potential differences between North America and Europe in the management and treatment of acute myocardial infarction.
Every week, you can expect clinical cases, expert opinions, polls and a selection of relevant resources on acute myocardial infarction, covering best practices from both sides of the Atlantic.
Check out the campaign here: AcuteCVDays (escardio.org)
Emergency care at crisis point
Lorna Rothery spoke to Jim Connolly, President of the European Society for Emergency Medicine about how long-established issues in the health system are being reflected in emergency care, and the bold actions needed to address this.
"Emergency medicine has faced unprecedented challenges over the past few years with ambulance offload delays, treatment delays and staff shortages. Would you say emergency medicine is being suitably prioritised as part of the EU’s public health agenda?"
Good question!!